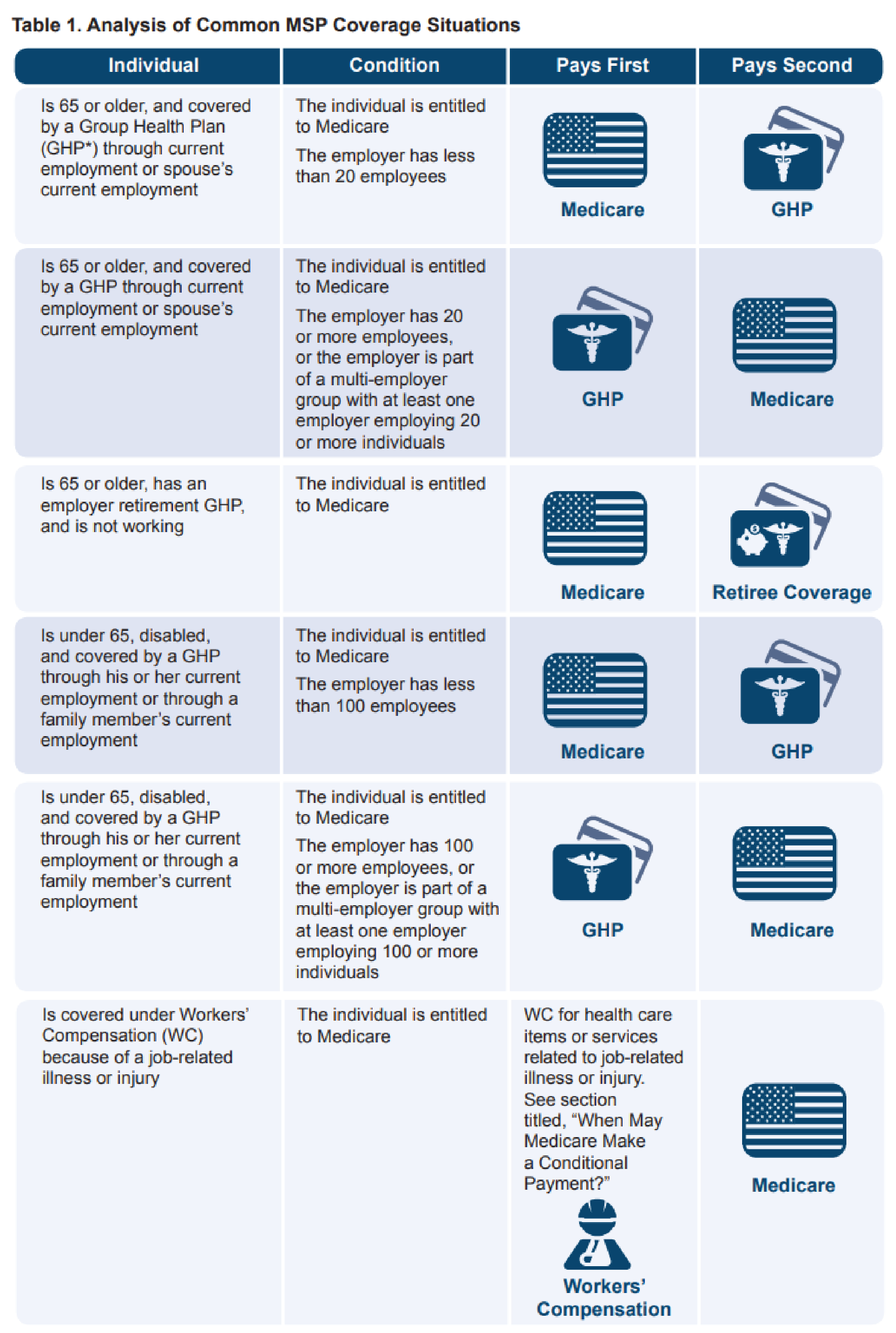
Medicare As Secondary Payer Fact Sheet - Since 1980, the medicare secondary payer (msp) provisions have protected. When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary payer,. Any entity providing items and. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. What is medicare secondary payer (msp)? Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment.
Since 1980, the medicare secondary payer (msp) provisions have protected. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. What is medicare secondary payer (msp)? Any entity providing items and. When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary payer,. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your.
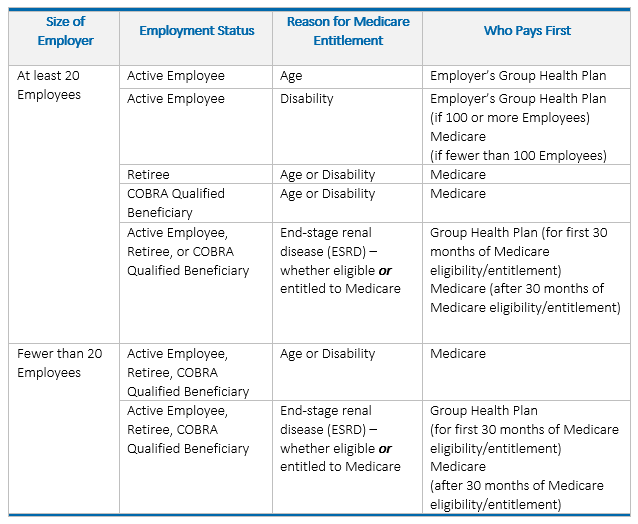
When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary payer,. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. Any entity providing items and. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. What is medicare secondary payer (msp)? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Since 1980, the medicare secondary payer (msp) provisions have protected.
PPT RHC BILLING 101 PowerPoint Presentation, free download ID1595196
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. Any entity providing items and. What is.
PPT Refinements to the CMSHCC Model For Risk Adjustment of Medicare
Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. What is medicare secondary payer (msp)? Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Any entity providing.
PPT Provider based billing PowerPoint Presentation, free download
What is medicare secondary payer (msp)? Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Since 1980, the medicare secondary payer (msp) provisions have protected. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. Any entity providing items and.
PPT Payers Module PowerPoint Presentation, free download ID3339547
Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Any entity providing items and. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. Providers, physicians,.
What is Medicare Secondary Payer? Ametros
Since 1980, the medicare secondary payer (msp) provisions have protected. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. When is.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
What is medicare secondary payer (msp)? Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Since 1980, the medicare secondary payer (msp) provisions have protected. Knowing what it means for medicare to be the secondary payer.
PPT McAnany, Van Cleave & Phillips, P.A. PowerPoint Presentation ID
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary payer,. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute.
Understanding Medicare Secondary Payer (MSP)
Since 1980, the medicare secondary payer (msp) provisions have protected. What is medicare secondary payer (msp)? Any entity providing items and. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary.
Overview of Medicare Secondary Payer Requirements Lyons Companies
Knowing what it means for medicare to be the secondary payer for health coverage can help you understand how your. Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate. Since 1980, the medicare.
PPT MSP Presentation Background & Basics Presented by Keith Ewing
Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. Any entity providing items and. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. What is medicare secondary payer (msp)?
Since 1980, The Medicare Secondary Payer (Msp) Provisions Have Protected.
Medicare secondary payer (msp) is the term generally used when the medicare program does not have primary payment. All medicare secondary payer (msp) claims investigations are initiated and researched by the msp contractor. When is medicare a “secondary payer?” in general, the group health plan is required to be the primary payer, and medicare is the secondary payer,. What is medicare secondary payer (msp)?
Knowing What It Means For Medicare To Be The Secondary Payer For Health Coverage Can Help You Understand How Your.
Medicare secondary payer (msp) provisions protect medicare from paying when another entity should pay first. Any entity providing items and. Providers, physicians, other suppliers, and individuals involved in the admission and billing procedures can contribute to the appropriate.